Cone beam computerized tomography for impacted teeth
Published: June 2016
Bulletin #56, June 2016
Cone beam computerized tomography for impacted teeth
Cone beam computerized tomography (CBCT) is used in dentistry today for several different diagnostic purposes, because it represents a giant leap forward as an imaging modality, by providing virtually unlimited 3-dimensional views of the teeth and the hard bony tissues that surround them. It does so with a relatively low radiation dose, far lower than that produced by spiral CT that is used in hospitals for full or partial body imaging and comes close to the levels involved in the taking of panoramic and cephalometric films. Progressive “slices”of the teeth and jaws in all directions at narrow intervals are routinely recorded to offer the facility to reveal differing consistencies of these tissues in health and in disease. It can ascertain the accurate anatomical configuration of the roots of teeth and of the alveolar bone and the proximity of a root to the inferior alveolar canal. It can measure the width of an alveolar ridge preparatory to implant placement, on a 1-to-1 basis, or the presence of alveolar bone supporting a periodontally involved tooth. It is a modality which serves every branch of the dental profession.
Since this website is concerned with the implications of the use of CBCT in the treatment of impacted teeth, we are concerned only with its relevance in relation to orthodontics and to the surgery that complements it and this will therefore be the frame of reference of the present discussion.
The relevance of CBCT to Orthodontics for Tooth Impaction:
The task of the orthodontist in any orthodontic treatment procedure is to plan the re-location of the teeth into their ideal/optimal/predetermined places in the dental arch, in alignment with the other teeth of the same jaw and in occlusion with those in the opposite jaw. This entire envisioned dental complex needs to be positioned in harmony with the hard tissue structures of the facial skeleton and the soft tissues of the lips, tongue and cheeks.
The discovery of an impacted tooth or teeth will complicate and lengthen the treatment of these cases.1 Such teeth are frequently to be found in ectopic locations and in bizarre orientations quite unlike other teeth, with their crowns often entangled in and around other structures, such as the roots of adjacent teeth and their roots, occasionally, encircling the inferior alveolar nerve bundle.
The fundamental and most important characteristic of a tooth is that it erupts from the site of its development within the alveolar bone into the oral environment “under its own steam”. Yet, the clinical approach of many orthodontists to an impacted tooth seems largely to ignore primacy of this basic fact! It frequently only comes to the fore, after many months of futile treatment, when what appears to be a straightforward impaction case fails to respond to an ostensibly efficient de-impaction mechanism. For a good many of these cases, the orthodontist will have omitted to ask the first and most crucial question “why has this tooth not erupted of its own?”, and has proceeded directly to treatment based solely on mechanical considerations. Certainly, there may be a supernumerary tooth, a small denticle, or other obstructive cause which may be obscured by superimposition of adjacent teeth in a 2-D planar film view. However, such entities as ankylosis, loss of contiguity of the lamina dura/PDL, invasive cervical root resorption (ICRR)2 and, rarely, pre-eruption intracoronal resorption (PEIR),3 are each highly likely to lead to an undermining of all attempts to move the affected tooth and are not always diagnosable with planar films alone. In order to see these pathologic lesions and to determine their character, the serial slices provided in cross-sectional, axial, coronal and longitudinal directions, achieved by good secondary reconstruction of the raw CBCT scan data, are essential (Fig. 1).
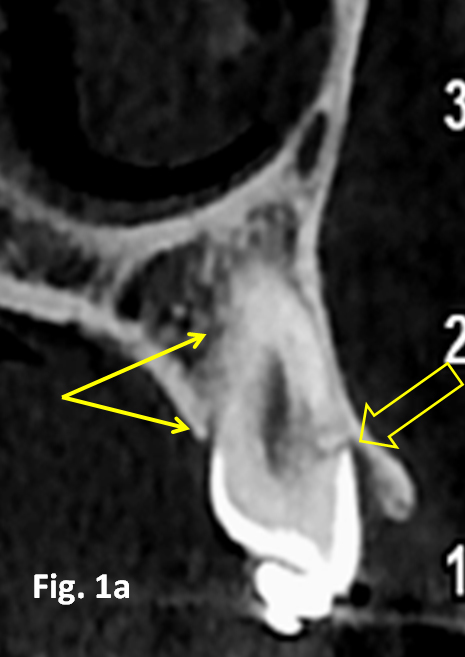
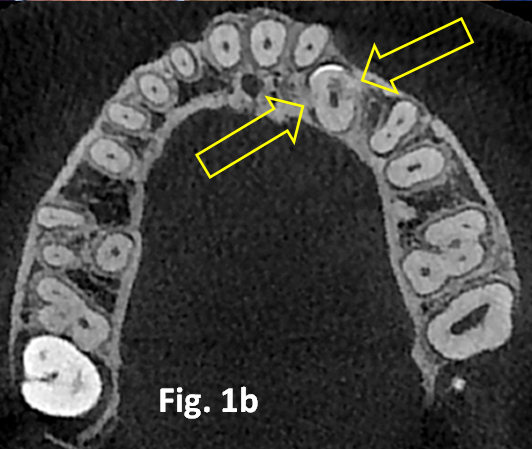
Fig. 1a. A cross-sectional view of an unerupted left maxillary canine shows 2 distinct areas of invasive cervical root resorption (ICRR) and their replacement with the deposit of new bone within the resorption lesion (arrows).
Fig. 1b. An axial slice from the same case illustrates the same 2 areas of cervical root resorption (arrows).
In the younger patient, the impacted tooth may have become arrested, but it may alternatively still exhibit eruption potential, with an aberrant eruptive direction that may further complicate its predicament and preclude its successful resolution. In a surprisingly high percentage of patients with an impacted canine, the proximity of the tooth will have caused active resorption of the root of the adjacent incisor4 and only active distancing of the tooth from the area will stop this destructive process.5
To be in a position to bring this impacted tooth into its place in the dental arch, therefore, a carefully planned directional traction strategy will be necessary to circumvent the obstacles that will otherwise impede its movement or exacerbate the resorption of the adjacent root.
To plan a potentially successful directional strategy, it is essential that the orthodontist be aware of the relations of the tooth to the surrounding structures, from crown-to-apex and along its entire length. This demands the use of 3-dimensional imaging and, for all but the simpler tooth impactions, the use of CBCT should be considered mandatory (Fig. 2 & 3).
For the orthodontist, the location of the apex of the tooth is more critical than the location of its crown, in terms of degree of complexity of the planned movement and prognosis of the outcome.8 If the apex is high, but in its ideal mesio-distal and bucco-lingual location – which occurs most of the time – then the essential components of directional traction are aimed at creating a tipping movement of the crown, together with extrusion and, possibly, a rotational element. On the other hand, if the apex and the crown are on the palatal side, then full resolution will require very considerable labial root torque, which will seriously lengthen the treatment time and reduce the periodontal prognosis.8, 10


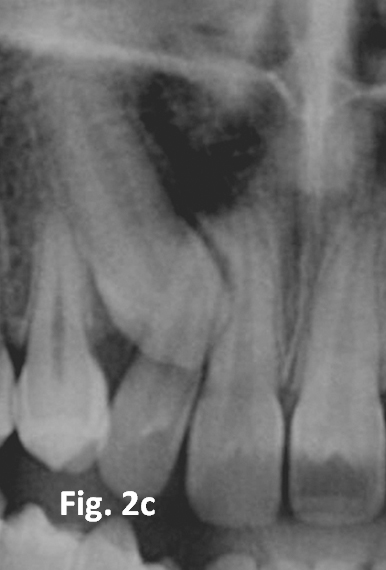
Fig. 2a. Panoramic view of a typical case with right maxillary canine impaction. The image of the canine superimposes on the middle of the root of the lateral incisor and, partially, of the central incisor. The fact that the canine image is enlarged, relative to the central incisor and compared with its opposite number, indicates that the tooth is palatally displaced.6, 7
Fig. 2b. The appearance and orientation of the canine on the anterior portion of the cephalogram confirms this tentative positional diagnosis.
Fig. 2c. Zooming the immediate area in the quest for root resorption. There appear to be no signs of root resorption.
Fig. 2d. See YouTube at https://youtu.be/9Q3nTQAWReM. A video clip of the same patient: Please follow the time scale at the bottom of the video. The first 10 seconds of the video clip provide an excellent demonstration of the tube shift method of locating the bucco-palatal relationship between the canine and the adjacent incisor roots. The initial view is directly from the front of the patient, is similar to the enlarged anterior portion of the panoramic view and shows the canine superimposed on the middle third of the roots of the central and lateral incisors. During the first 6 seconds of the video, the tube rotates to the right around the patient’s head and the canine is seen to “move away” from the central incisor to remain superimposed only on the lateral incisor. At the 13 second mark and with the gradual establishment of a true lateral view, the tooth becomes “separated” from the incisor root entirely, with the crown of the canine clearly lingual to the line of the arch palatal to the incisors. At 35 seconds, the teeth are viewed from the lingual and the roots of the premolars are oriented with a slight distal crown tip. The palatal root of the first premolar can be seen to be in close relation with the CEJ of the underside (distal) of the canine. Any distal tipping designed to create space for the canine in the dental arch will obviously tend to throw the root apices of the premolar mesially, against the root of the canine and block the eruption path of the canine. Using a coil spring squeezed between labial brackets to increase space will also tend to rotate the premolar and this will have the effect of rotating the palatal root mesially, to further impede the canine eruption path.
If the picture is now complicated by the presence of the lateral incisor root lying in the direct path between the crown of the palatal canine and its place in the arch, this obstacle will need to be circumvented by a downwards and posteriorly-directed movement first, before the tooth may be drawn towards its intended location.
Similarly, when a first premolar is mesio-buccally rotated and its palatal root has a mesial curvature or bend in it, the apex of this root may often lie directly in the path of the canine and it might be labial to it or lingual to it. This will be very difficult or impossible to distinguish on panoramic or periapical radiographic views alone, even when supplemented by other planar views. Corrective action to free the canine needs to be undertaken by rotating or over-rotating the premolar so that its palatal root is turned away from the canine, as well as over-uprighting the tooth distally, to further distance the root apex.11
There are many instances with canines in which the initial direction of traction cannot be aimed towards the prepared space in the dental arch in the immediate post-surgical period because of these and other obstacles that may intervene to block the direct route. When a circuitous route needs to be planned, placing an attachment in the mid-buccal location of the crown of the tooth will generate a superfluous rotational moment, when traction is applied. So, the initial direction of traction dictates the preferred location of the attachment on the crown of the tooth and this must be planned ahead of time.
The accurate diagnoses of all these situations (and many more) can find their solution in CBCT imaging, in which a single circuit of the cone around the patient’s head is sufficient to provide all the information described above.
From this, we may conclude that when the orthodontist talks about diagnosis in relation to impacted teeth, there are two aspects to consider. The first relates to why the tooth has become impacted (pathology or obstruction), for which the CBCT examination must include the preparation of a progression of slices of the affected area in the axial, cross-sectional, coronal and longitudinal planes at intervals of 0.5-1mms. The second refers to the 3-dimensional location of the tooth within the jaw and its relation to the immediate surrounding structures within which it may be entangled and from which it requires to be extricated. The manner of its impaction is best understood and an operative plan for its resolution best formulated with the help of 3-dimensional CBCT views in all directions, generated from the secondary reconstruction of the raw data into the form of a video clip or, at the very least, a good number of individual 3-D screen shots seen at different angles and from varied vantage points.


Fig. 3a. A view of the dentition from the front of a 13.6 year old male, showing absence of the left maxillary central incisor and labially ectopic permanent canines. The partially erupted tooth in the central incisor location is a midline supernumerary tooth of poor form.
Fig. 3b. The relevant portion of the panoramic film shows 2 supernumerary teeth, the left impacted central incisor and the abnormal orientation of the left lateral incisor. In some cases, difficulty of aligning a much displaced permanent incisor may make the orthodontist look to the possibility of extracting it and aligning the supernumerary in its place.
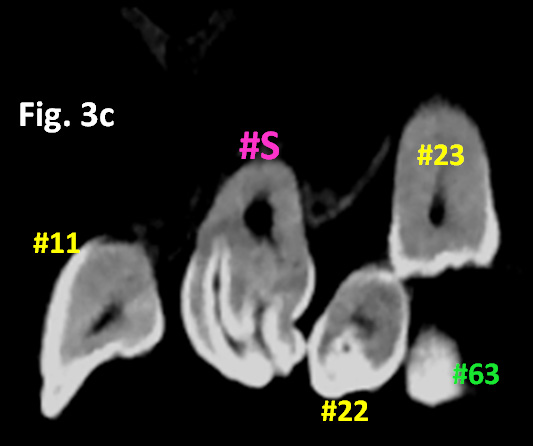
Fig. 3c. A longitudinal and oblique cut from the secondary reconstruction of the CBCT data across the anterior teeth shows the unsuitability of preserving the supernumerary tooth (#S), due to its convoluted crown and short root. Note also the dens in dente in the lateral incisor (#22).
Fig. 3d. See YouTube at https://www.youtube.com/watch?v=eDsnnMwIn2Y. A video clip of a patient illustrates 2 maxillary median supernumerary teeth causing eruption disturbance of the left central and lateral incisors and the adjacent canine. One is small and conical and unerupted high on the labial side. The second is large and partially erupted. The central incisor is rotated 180o, with its crown tipped lingually. The lateral incisor is erupted, with its crown in its normal location but the orientation of its root proceeding apically on a lingually and distally displaced axis. The deciduous canine is still in place, although its root has completely resorbed and its over-retention has contributed to a labial ectopic displacement of the permanent canine. By replaying this video clip several times, positional diagnosis of the location and inter-relation of these teeth can be easily identified and the appropriate surgical episode approached with well-founded confidence.
The relevance of CBCT to Oral Surgery for Tooth Impaction:
For the orthodontist to be in a position to positively influence and control the eruption of a buried tooth, it is necessary to provide access to this tooth and to place some form of attachment on it, by means of which forces may be applied. Thus a surgical procedure needs to be undertaken, during which an area of exposed enamel of the crown of the tooth is exposed and isolated, in preparation for acid-etch attachment bonding. The surgeon’s role is limited to this singular purpose, since he/she has little control of the subsequent progress of the tooth’s eruption and none at all in controlling its direction. These functions are entirely within the realm of orthodontics and dependent on the orthodontist’s skill and inventiveness in planning the appropriate direction, range and force values. Indeed, excessive surgical involvement in over-extensive exposure of the tooth down to and beyond the CEJ and instrumentation of the cementum of the root may cause irreparable damage, in the form of gingival recession with an unesthetic long clinical crown or by initiating such pathologic entities as invasive cervical root resorption and ankylosis.
Assuming proper 3-dimensional positional diagnosis of the tooth and commensurate planning of the movements needed for its resolution on the part of the orthodontist, the oral surgeon only requires to know the exact location of the crown of the tooth. The length, shape and orientation of the root and its relationship to adjacent structures are irrelevant for the immediate surgical episode. While this is true of the impacted tooth, it should be remembered that surgical access to the tooth may be blocked by the presence of one or more supernumerary teeth or odontomes, which will need to be extracted. Furthermore, access may be limited by the proximity of the roots of adjacent teeth, particularly when these have suffered resorption. So the oral surgeon is less concerned with root displacement and other technical difficulties in resolving the impaction of the tooth and more interested in limiting the trauma that must accompany every surgical procedure, in the quest to provide good access for attachment bonding.
In my experience with a number of oral surgeons, with whom I interact in these circumstances, I have noted that they are likely to be more interested in the serial slices provided in cross-sectional, axial, coronal and longitudinal directions by good secondary reconstruction of the raw CBCT scan data. However, the ability to see a 3-D screen shot or video clip of the surgical field provided by the cone beam technology, before the patient reaches the operating theater, offers an excellent basis for the essential discussion of the specific aims and requirements of the procedure between orthodontist and oral surgeon ahead of the procedure.
Norms in the use of CBCT various countries
I had hoped to present the details of an internet survey among the regular subscribers to this website which I circulated to the full roster of orthodontists in my address book (approximately 1500 colleagues worldwide) a couple of months ago. Unfortunately, the number of colleagues who returned completed questionnaires was too small to offer any reliable insight into the manner in which orthodontists use the modality.
References:
1. Becker A, Chaushu S. Success rate and duration of orthodontic treatment for adult patients with palatally impacted maxillary canine. American Journal of Orthodontics and Dentofacial Orthopedics. 2003;124:509-514.
2. Becker A, Abramovitz I, Chaushu S. Failure of treatment of impacted canines associated with invasive cervical root resorption. Angle Orthodontist, 2013;83:870-876.
3. Becker A, Chaushu S. Impacted teeth and the 6 incarnations of resorption. (Les six formes de résorption associées à l’inclusion dentaire). L’Orthodontie Francaise, 2015;86:277–286).
4. Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. American Journal of Orthodontics & Dentofacial Orthopedics, 2005;128:418–23.
5. Becker A, Chaushu S. Long-term follow-up of severely resorbed maxillary incisors following resolution of etiologically-associated canine impaction. American Journal of Orthodontics and Dentofacial Orthopedics 2005, 127: 650-654.
6. Chaushu S, Chaushu G, Becker,A. The use of panoramic radiographs to localize maxillary palatal canines. Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endododontics 1999; 88:511-516.
7. Chaushu S, Chaushu, G, Becker A. Reliability of a method for the localization of displaced maxillary canines using a single panoramic radiograph. Clinical Orthodontics and Research 1999; 2:194-199
8. Becker A, Chaushu S, Casap-Caspi N. CBCT and the Orthosurgical Management of Impacted Teeth. Journal of the American Dental Association 2010;141(10 suppl):14S-18S.
9. Becker A, Kohavi D, Zilberman Y. Periodontal status following the alignment of palatally impacted canine teeth. American Journal of Orthodontics,1983;84:332-336.
10. Kohavi D, Becker A, Zilberman Y. Surgical exposure, orthodontic movement and final tooth position as factors in periodontal breakdown of treated palatally impacted canines. American Journal of Orthodontics, 1984;85:72-77.
11. See http://dr-adrianbecker.com/page.php?pageId=281&nlid=22. December 2011 bulletin #6 on this website



