Rescuing Teeth Impacted in Dentigerous Cysts
Published: April 2014
Bulletin #32- April 2014
Rescuing Teeth Impacted in Dentigerous Cysts
A number of years ago, I had the good fortune to have been asked by one of the leading orthodontic journals to review a manuscript reporting a case in which several teeth were widely dispersed and impacted within and in the wall of a very large dentigerous cyst. The lesion occupied and expanded until it had resorbed away a large volume of the right side of the maxilla, displacing the canine to a location near the floor of the orbit. The outcome of the treatment was elimination of the cyst and complete alignment of the involved teeth.
At the time, it initially seemed to me that the article had been presented as a “wow” article to flaunt a one-off astonishing treatment that had worked out unbelievably well, as if by chance. It therefore had sensational news value, in line with the type of “man bites dog” headline that one is more likely to see in a yellow tabloid newspaper.
I recognized that the treatment provided for the patient in that article followed sound scientific principles, based on knowledge of histopathology and oral surgery and, thus, not well known in our specialty. I considered that, bringing it to the attention of the orthodontist, who could well be called upon to treat a case of this type – rare though it might be - was an important priority and I recommended that it be published in the journal. The article opened my eyes to the degree of autonomous correction of the ectopic location of teeth that is possible and reasonable to expect following the resolution of dentigerous cysts, in general.
A word about etiology:
The etiology of dentigerous cysts is not clear, although they are often associated with the longtime presence of a chronic granuloma related to a non-vital deciduous predecessor. It seems that the granuloma acts as an irritant to the adjacent follicle of an unerupted permanent tooth. These cysts are slow-growing, spherical, space-occupying lesions within bone, whose origin is in the enlargement of the dental follicle. Thus, they surround the clinical crown of the unerupted tooth, the orientation of whose long axis crosses the perimeter of the sac at 900 to the curved surface of the cyst, always pointing to its epicenter. They are filled with a sterile fluid and are entirely symptomless, unless they become secondarily infected. As they grow in size, the intra-cyst pressure builds up until it overcomes the eruptive force of the included tooth. From that point on, the tooth slowly backs up along its former eruption path. Alveolar bone is resorbed as the cyst enlarges and new bone is compensatorily deposited on the outer surface of the maxilla, but at a slower rate. Thus, the alveolar ridge will become broadened, altering its shape in the labial and buccal sulcus and palatal areas, while the bony periphery becomes progressively thinner.
Although making little difference in clinical terms, the dentigerous cyst needs to be differentiated from the radicular cyst. The radicular cyst behaves in an almost identical manner with the exception that it is thought to arise from the epithelial rests of Malassez that are to be found in the apical area of a tooth and which are stimulated into the formation of the cyst by the presence of a chronic granuloma in the immediate vicinity. The granuloma is associated with a non-vital tooth which, in the anterior region, is often the result of trauma to a deciduous tooth which was left untreated or remained unresolved by an inadequate root canal procedure. The cyst adopts all the features of the dentigerous cyst, with the exception that the adjacent teeth will be displaced against the extremity wall of the cyst, in different directions and none will be within the cyst cavity.
Presentation:
Unless the cyst becomes infected, its discovery is usually serendipitous, since there is no pain. In the incisor region, it most commonly follows the complaint of the parent of an 8 year old child that there is a discolored and over-retained deciduous central incisor on one side, while the two contralateral permanent incisors have erupted. When associated with other teeth, its discovery will be correspondingly later. Perceptible facial swelling and asymmetry will occur only when the cyst is very large. The intra-oral picture is quite typical, with an alteration in the concave palatal vault which exhibits a convexity on one side. On the buccal/labial side of the alveolar ridge there is a complementary and distinct swelling extending into the height of the sulcus.
When the young patient is seen by an orthodontist whose experience with this entity is limited, the diagnosis is unlikely to be obvious, based purely on a clinical examination. Perhaps the most characteristic feature is seen on the panoramic radiographic view. Depending on the size of the cyst, the teeth in the immediate area will be seen to have been pushed aside and dispersed in all directions, with a radiolucent void between them. The canine will often be displaced high in the maxilla beneath the orbit, with the lateral incisor lying almost horizontally, low down and just above the roots of any over-retained deciduous teeth.
Naturally, a CBCT series will provide excellent imaging of this lesion in the 3 planes of space. However, at this point, it is entirely superfluous, since the accuracy of the plane film imaging is adequate to establish the diagnosis and additional 3D positional information will not change the approach to treatment. The initial phase of treatment is solely aimed at eliminating the pathologic entity, i.e. the cyst. As a by-product, cyst resolution will generate spontaneous and radical improvement in the positions of the individual teeth ahead of any biomechanical attempts to resolve their extreme ectopy. Indeed, the changes are often so far-reaching that the CBCT will contribute nothing to the later planning of orthodontic alignment of the teeth. If CBCT is necessary in these cases, it will only offer any relevance if it is executed after the complete elimination of the cyst and after bony fill-in of the defect. At that point, surgical exposure of the individual impacted teeth will be necessary and a plan for appropriate directional traction will need to be determined. It is only then that accurate 3D positional information will be required.
Treatment:
Before the orthodontist may even consider including the teeth impacted within or adjacent to a dentigerous cyst in the overall treatment plan, he/she must know whether these teeth are salvageable with a good prognosis. This means that the pathology must be eliminated and the involved teeth must be brought into the arch and evaluated in terms of the health of their supporting structures, i.e. alveolar bone height and quality of the regenerated alveolar bone, the periodontium, clinical crown length and appearance. Alternatively they must be extracted before other treatment considerations may be contemplated. In the oral surgical literature, elimination of the cyst is performed in one of two ways. Careful enucleation of the lining of the cyst is often preferred by oral surgeons, because of the remote possibility of neoplastic change in its epithelial lining. However, with larger cysts, their proximity to the inferior alveolar nerve canal creates a serious risk of collateral damage – not to mention the likelihood of the loss of associated teeth.
Marsupialization is the alternative method, which involves decompressing the cyst by creating a relatively small surgical opening into it at a convenient site and maintaining this opening or stomium until there is bony fill-in behind the cyst lining, which is deliberately left in place. The included teeth are not exposed but remain covered by the cystic lining. As fill-in occurs over the subsequent months, the teeth are carried forward as if on the crest of a wave and their positions, improve until they come together from their former widely ectopic locations. In a good proportion of cases, some of the teeth will erupt spontaneously. The cystic lining shrinks with the advancing osteogenesis and, with the eruption of the teeth, eventually undergoes metaplasia as it merges with the oral mucosa. This mechanism is arguably anomalous with the normal eruption of teeth and the merging of the reduced enamel epithelium of a normal dental follicle with the gingival tissues.
Following marsupialization, there is a period of between one and two years during which the cyst is eliminated as bony regeneration progresses. This needs to be monitored with periodic periapical radiographic follow-up until orthodontic treatment may be commenced, as indicated by the teeth coming together. The radiographic monitoring should also take into account the remote possibility of neoplastic change of the epithelial lining.
Surgical exposure and active attempts at orthodontic traction with bonded attachments on the teeth before this time are strongly contraindicated, since their supporting bone and periodontium are very sparse and underdeveloped. Patiently waiting for the fullest expression of autonomous correction that is forthcoming will be rewarded by a shorter and more successful orthodontic treatment phase.
Once there is evidence of consolidation of the bone around the impacted teeth, surgical exposure of the teeth that have not erupted may be undertaken with relative simplicity, due to their vastly improved positions and orthodontic traction may be applied to erupt them into the mouth.
With the previously impacted teeth erupted in the mouth and before alignment is attempted, a re-evaluation of the case as a whole should be undertaken in the normal way, having now ascertained the prognosis of the individual teeth.
An approach to the biomechanics of aligning the teeth and achieving an acceptable clinical outcome in these cases will be the subject of a future bulletin.
Case #1*
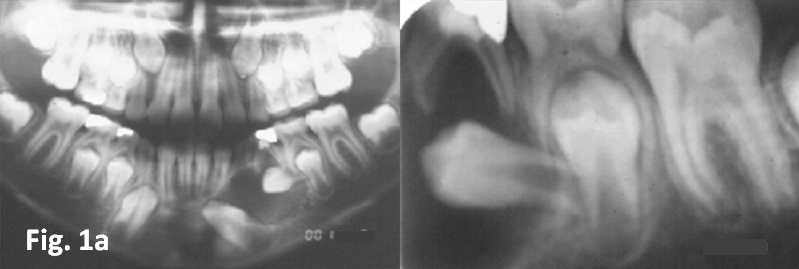
Fig. 1a represents panoramic and periapical views of a large cyst associated with the non- vital deciduous first mandibular molar, which had had root treatment with incomplete resolution. Differential diagnosis is academic, but it may be a radicular cyst arising from the periapical granuloma of the deciduous molar or alternatively a dentigerous cyst arising from enlargement of the follicle of the unerupted first premolar, initiated by the local infection at the deciduous molar.

Fig.
1b. presents an interim periapical view of the immediate area 2 months after
marsupialization of the cyst. Note the spontaneous improvement of the
orientation of the permanent canine and first premolar. 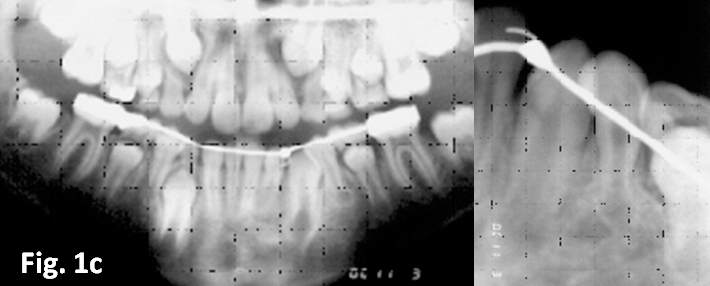
The panoramic and periapical views of the case 10 months after surgery is presented in Fig. 1c, showing total resolution of the cyst and full eruption and spontaneous uprighting of the affected teeth.
Case #2*
The cyst occupies most of the right side of the maxilla and is related to the non-vital deciduous central incisor seen in the first 3 slides. The panoramic film is a rotational tomogram and because the central incisor is grossly displaced close to the floor of the orbit and outside of the focal trough (Fig. 2a), the tooth is not visible. The tooth is however clearly seen on the anterior occlusal view (Fig. 2b). Fig. 2c is an annotated copy of Fig. 2a, to show the extent of the cyst (red dashed elipse) and how it has displaced the canine into the area of the second molar. The lateral incisor and both premolars have been pressed downward by the hydrostatic intra-cystic pressure to lie horizontally in the floor of the cyst. Fig. 2d is the same case 20 months after the decompression surgery to show how the elimination of the cyst by marsupialization has brought the widely dispersed teeth together with the regeneration of alveolar bone behind them. Coincidentally, the premolars have spontaneously uprighted. At this point, orthodontic treatment was commenced and the teeth exposed, to attempt to resolve the impactions and to bring the teeth into good alignment and function.
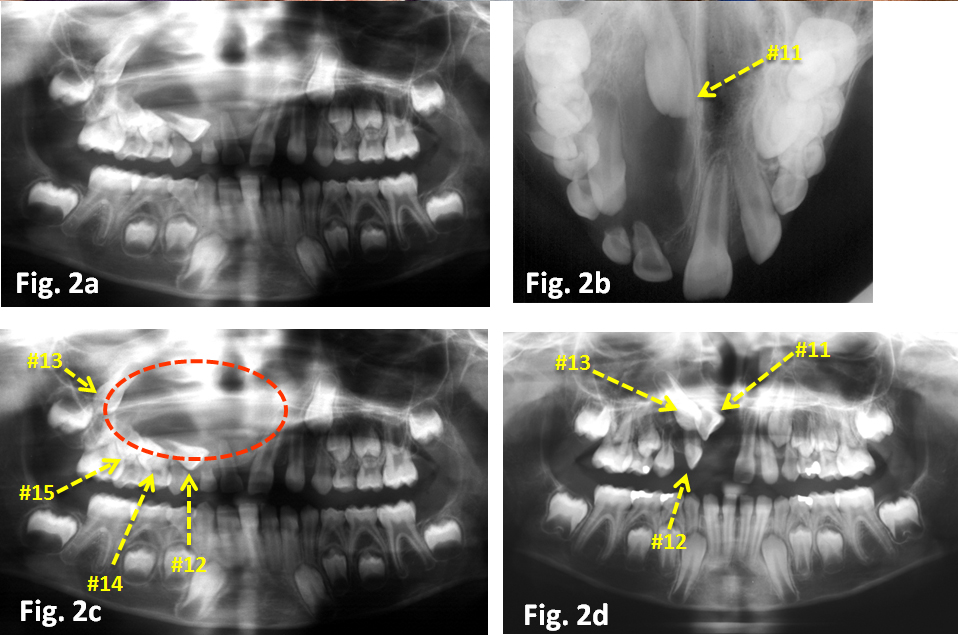
Case #3*
As with case 2, the trigger for the development of
the cyst was the untreated necrotic pulp of the deciduous central incisor. Fig.
3a is the intra-oral clinical photograph of the anterior teeth, showing the
discolored incisor. It also shows the extreme expansion of the alveolar bone of
the sulcus and the blue tinged mucosa indicating an extremely thin bony wall.
The degree of dispersion of the unerupted permanent teeth in the walls of this
very large cyst can be seen to be similar to the earlier case. As can be seen
in a-p cephalogram, the ENT surgeon’s film directed at the sinuses and the
lateral cephalogram (Fig. 3c-e), the canine in particular is displaced in the
lateral, vertical and sagittal planes. 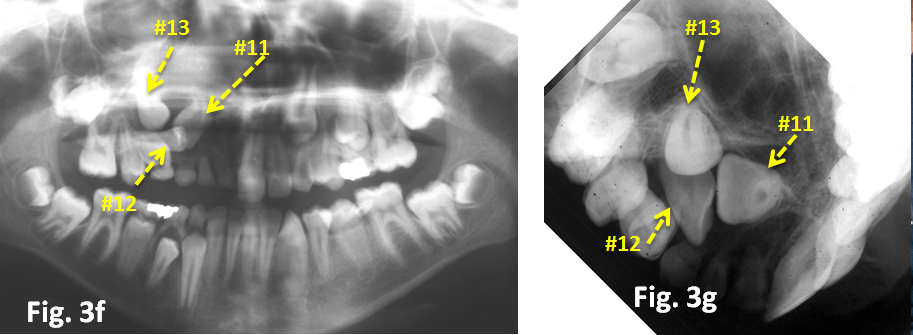
At 39 months after decompression had been performed by simply draining the cyst into the mouth and maintaining the opening until the cyst lining and oral mucosa had fused together, the entire cavity filled up behind the former cyst lining, carrying the teeth forward as on the crest of a wave. Further spontaneous improvement did not occur and orthodontic treatment was instituted to complete the case. This will be described in a future bulletin.
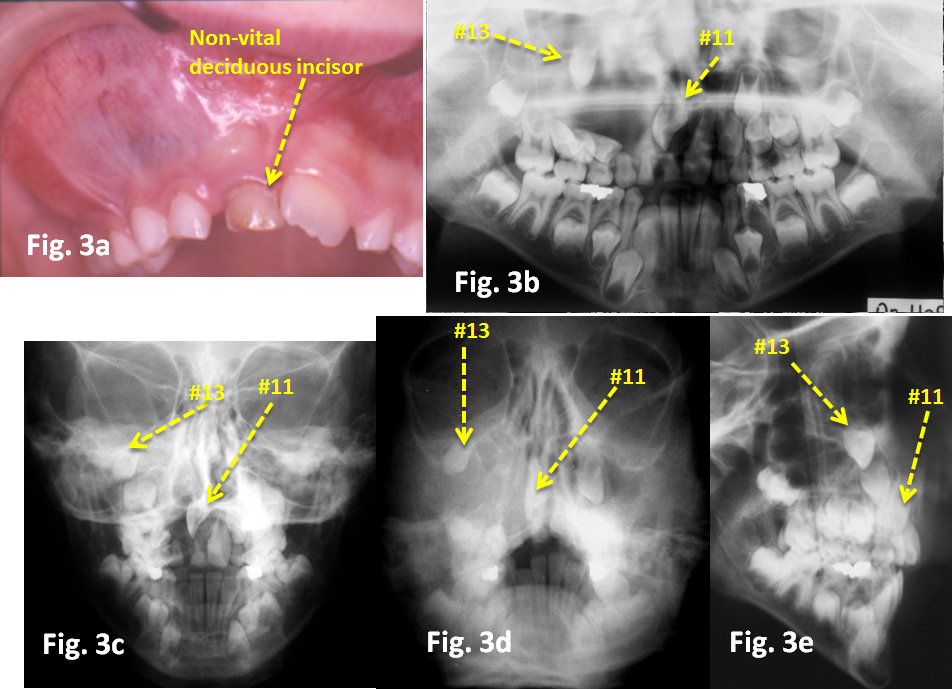
Case #4*
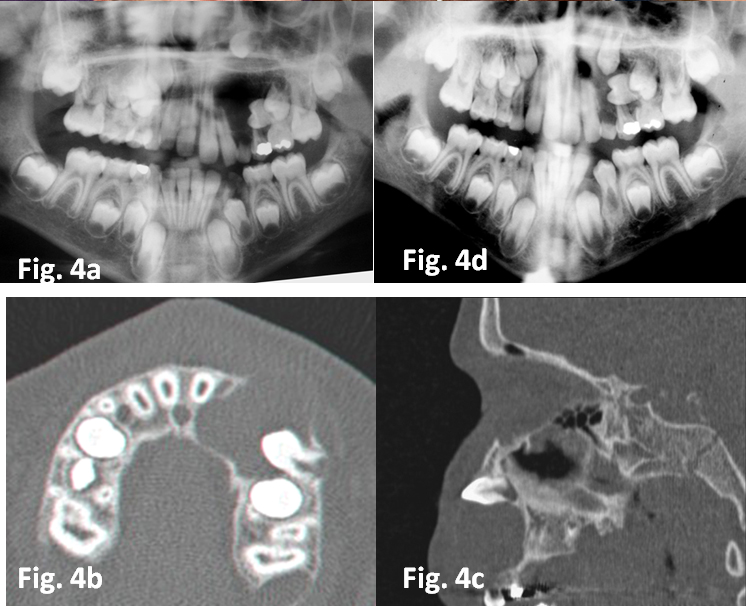
The very large cyst in this case (Fig. 4a) is more
distally located and has probably been initiated by the non-vital first
deciduous molar. The canine and the two
premolars lie flat in the walls of the cyst and the hydrostatic pressure has
pushed the canine up to the floor of the orbit. The CBCT axial (Fig. 4b) and
transaxial (Fig. 4c) cuts shown here clearly outline the borders of the lesion
and illustrate the degree to which the bony wall expands and become paper thin
both buccally and palatally. Fig 4d shows how much regeneration has occurred at
5 months after marsupialization of the cyst. A maxillary holding arch was
placed to at this time and the patient was recalled periodically as a routine
follow-up. At 26 months pot surgery, the formerly impacted canine and premolars
were beginning to erupt and the panoramic view taken at that time (Fig. 4e)
showed excellent progress. It also showed that the right canine had developed a
fairly extensive dentigerous cyst and this was drained together with extraction
of the deciduous canine and first deciduous molar on that side.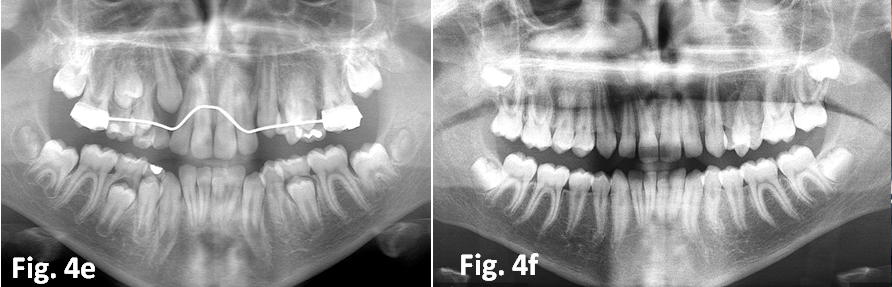
Seen 26 months later, all permanent teeth had erupted fully and orthodontic treatment was initiated for some very minor malalignments. The extreme severity of the initial condition had resolved itself with only the most minor of surgical interventions and no orthodontics.
*The cases illustrated here are copyright and largely taken from
Becker A. Orthodontic Treatment of Impacted Teeth. 3rd edition. Oxford: Wiley-Blackwell Publishers, 2012.



